Treatments
Botox for Migraines

OnabotulinumtoxinA, also known as Botox has been found to be successful in the treatment of Chronic Migraines. How does it work? Botox is a neuromuscular blocker which means it paralyses the muscle into which it is injected.
Botox works for migraine headaches because it blocks chemicals called neurotransmitters that carry pain signals from the brain. Botox is like a roadblock in that pathway. It stops the chemicals before they get to the nerve endings around the head and neck.
It was once used by doctors for cosmetic purposes, such as smoothing out wrinkles; however, today it’s been found to be useful in the treatment of several medical disorders, including crossed eyes, cerebral palsy, tics and chronic migraines.
Occipital Blocks
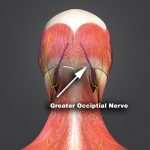
Chronic Headaches, Neck or Head Pain, and Occipital Neuralgia:
Whether you suffer from chronic headaches, Occipital Neuralgia or just pain in your head or neck, you may be a candidate for Occipital Nerve Blocks. What is it and how does it work?
An Occipital Nerve Block is an injection of a steroid or other medication around the greater and lesser occipital nerves that are located at the back of the head, just above the neck. A small needle is inserted just under the skin and deeper tissues, after the area is numbed with a local anesthetic. Then a steroid medication is injected into the deeper tissues.
Once the medication penetrates the nerves, it’s meant to reduce the inflammation and swelling around the nerves that was causing the pain in the first place. It can take up to 3-5 days before results are seen. Some patients require more than one injection before they experience relief, typically returning a few times for weekly or bi-weekly injections.
Injection Therapies

Trigger Point Injections (TPI)
Muscles containing trigger points can sometimes irritate the nerves around them and cause pain in different parts of the body. TPI’s can be used to treat muscle groups in the arms, legs, back and neck. Persons suffering from Tension Headaches and Fibromyalgia may also benefit from Trigger Point Injections.
Trigger Point Injection (TPI) is a procedure where a single injection is made in a person’s trigger point, sometimes at multiple sites on, near and around the muscles containing trigger points. The injections can consist of certain anti-inflammatory medicines or in some instances, no medication at all (also known as Dry Injections), causing the trigger point to become inactive, alleviating the pain. Some patients benefit from just one round of TPI’s, others require a few rounds of treatment before they experience relief.
Cortisone Injections
These injections are comprised of a corticosteroid medication and a local anesthetic and are usually injected at a joint. The injection is used to help alleviate pain and reduce inflammation. Many conditions can be treated with cortisone injections, including plantar fasciitis, tennis elbow, bursitis, tendonitis, gout and certain arthritic conditions. The most common joints that are treated with cortisone are: the shoulder, elbow, hip, knee, wrist and spine.
Peri-Neuro Injection Therapy
Perineural Injection Therapy (PIT) is a proven safe, effective treatment for patients who may not be candidates for joint replacement surgery or biologic options such as PRP or Stem Cell. Perineural injection therapy treats inflamed and injured nerves. When a nerve becomes inflamed it can release chemicals which in turn cause inflammation, pain, and tenderness. By injecting a small amount of Dextrose and Water into the nerve with a small needle, the nerve is calmed almost instantaneous and symptoms dissipate.
Chronic nerve pain is often due to trauma, arthritis, sports injuries, occupational stresses on the body, and surgical injuries.
Most patients require 4-6 Perineural Injection Therapy treatments spaced anywhere for 7-10 days to 2-4 weeks apart depending on their condition.

Spine Injections
Epidural Steroid Injections (ESI)
There are several types of these injections, each slightly different in their methodology to treat the spine and affected areas; however, the process is similar in each approach. A needle is passed through the skin, subcutaneous tissues and spinal ligaments, and into the epidural space. Three common types of ESI’s we practice are caudal steroid injections, transforaminal steroid injections and lumbar steroid injections.
Transforaminal Epidural Steroid Injection
With this approach, the needle is placed by way of fluoroscopy into the foramen, which is where the nerve root exits the spine to both the left and right side. The candidates that are best served with this injection are patients who experience most of their pain in a lower or upper extremity rather than just in the spine.
Caudal Epidural Steroid Injection
A needle is inserted into the epidural space at the lowest point. Using fluoroscopy to properly place the needle, a local anesthetic is used in conjunction with a corticosteroid to help reduce inflammation, which in turn is meant to reduce or alleviate pain.
Facet Injections
Two facet joints are located behind every two vertebrae at the back of the spinal column, each for the purpose of allowing the body to bend, twist and make movements. Where one facet joint connects to another there is a cartilage cover and a synovial cover, aiding the spines movement whilst avoiding friction. When a facet joint becomes inflamed, whether due to osteoarthritis or other degenerative disc disorders, it may cause pain. A facet injection can be used to diagnose and/or treat facet joint disorders.
Knee Injections

Hyaluronic Acid Injections for Knee Osteoarthritis
There are several different types of hyaluronic acid injections used to treat knee osteoarthritis; some include Supartz, Supartz FX, Synvisc, Monovisc, and Orthovisc. Hyaluronan is a natural chemical that’s found in the body near joints, usually in the tissues and synovial fluid. Hyaluronic Acid is much like the Hyaluronan chemical found naturally in the body. This injection is great to help aid in lubricating the knee joint, enabling people with Knee Osteoarthritis to resume physical activities.

Regenerative Medicines
Platelet Rich Plasma (PRP)
In recent years, athletes have turned to PRP therapy to treat their damaged tendons and muscle sprains. Today, doctors are using PRP to treat chronic pain, arthritis, joint pain, back injuries and much more. The use of concentrated growth factors is considered by many to be an exciting new cutting edge therapy that can stimulate tissue repair, and regenerate weakened, torn or damaged ligaments and joints. Platelet Rich Plasma (PRP) is a concentration of platelets and growth factors created from a small amount of blood or bone marrow extracted from a person’s body.
How Does It Work? A small amount of blood or bone marrow is taken from a person. That sample is then put into the Angel PRP System, which spins the blood, separating the plasma from the blood, in small concentrations; the process takes about 30 minutes. Once the plasma on its own, it’s injected directly back into the patient, allowing the body to heal itself with its own stem cells and blood platelets.
Platelet Rich Plasma (PRP)
Prolotherapy is a non-surgical treatment option for persons who suffer from joint and ligament disorders including arthritis, knee injuries, tendinitis, spine disorders, ACL tears, and rotator cuff injuries.
An injection is given at the injured or weakened areas of the body with a solution that stimulates the growth of healthy, strong tissues. As the tendons and ligaments grow stronger, the body begins to regain active range of motion, and pain dissipates.
Stem Cell Therapy
Blood collected from the umbilical cords of healthy newborn babies, can in turn be used to help regenerate and restore health to persons with back and neck conditions, joint and cartilage injuries and has even been used to treat immune system disorders and blood diseases.
